1 Introduction
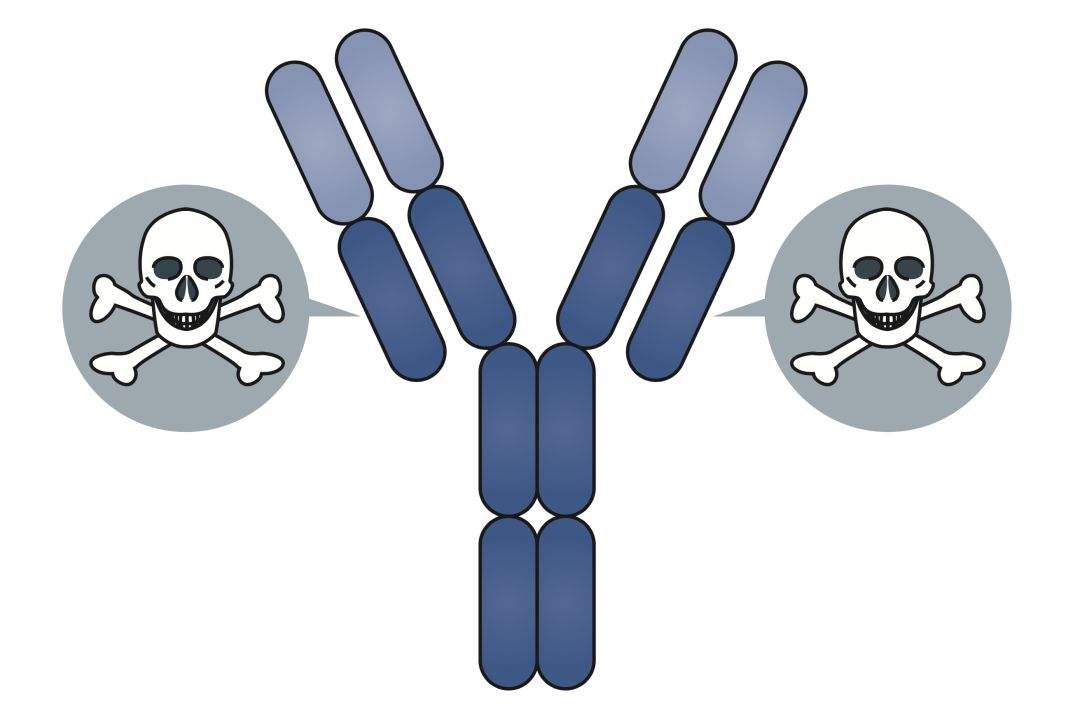
First, a brief introduction to the composition of ADC drugs, antibody-drug conjugates, as the name suggests, includes 3 partial antibodies, drugs (also known as drug carriers, drug or payload, small molecule toxins), and linkers (linker, linker). The general mechanism of action is that the antibody leads the ADC to the target site through its specific affinity with the target site antigen, and the ADC bound to the antigen is endocytosed into the target cell, and then a cytotoxic payload is released in the cell, and then The target cells are killed to exert their effects.
Since ADC drugs are different from monoclonal antibody drugs, they are generally administered by IV, and there is almost no SC administration, so this article will not discuss the absorption characteristics of ADC drugs, so as to introduce the theoretical knowledge of the distribution and elimination of ADC drugs. (The reason why ADC is not administered subcutaneously: After the ADC drug is administered by SC, in order to pass through the blood vessel wall from the intercellular space at the injection site to reach the plasma, the lymphatic system or neonatal Fc receptors must be used. can cause toxicity to lymphoid organs, thus limiting subcutaneous administration of ADC drugs)
2 Distribution of ADC drugs
The main body of the ADC drug structure is still the antibody part, so its distribution characteristics are basically similar to those of naked antibodies. The factors affecting the drug distribution of ADC mainly include three aspects: target-mediated specific distribution, plasma, tissue fluid and lymph. Convective fluid flow, the nature of ADC drugs.
First, the target-mediated distribution process is introduced, which is mainly affected by the expression of the target antigen and the rate of endocytosis. In theory, as long as it is a tissue that expresses the target antigen, whether it is a normal tissue or a lesion tissue, ADC drugs will be attracted to it. For normal tissues, the release of the payload after the ADC drug runs over will cause toxicity. Therefore, selecting a suitable target antigen is particularly important for the therapeutic window of the ADC drug. The expression of the target antigen must be sufficiently different between tumor tissue and normal tissue. .
The higher expression of target antigens in normal tissues will also affect the drug distribution into tumor tissues due to competition and affect the efficacy of drugs. Some people have imagined why not to use naked antibody to occupy the target antigen of normal tissue in advance, and then give ADC drug to avoid ADC exposure of normal tissue and avoid toxicity. I have to say that this idea is really attractive, but There are also many limitations to the feasibility of this idea. For example, how much naked antibody should I give first to ensure that while saturating the target antigen of normal tissue, the target antigen of tumor tissue will leave some blanks for subsequent ADC drugs, otherwise ADC drugs will not be useful down.
The variability of target antigen expression among individuals, in turn, may lead to different individuals may require different naked antibody doses, which brings a head-on to the implementation of this idea. In addition, naked resistance is not a waste, it can also exert pharmacological activity itself, which complicates things, so this strategy can only stay in the mind. Second, the effect of fluid convection of plasma, interstitial fluid and lymph on ADC drug distribution. Since the molecular weight of ADC drugs is generally around 150kDa, such a behemoth naturally cannot shuttle back and forth freely like a small molecule, so it can only stay in the blood vessels for a short time after administration, so its distribution volume is basically the physiological volume of plasma The level is generally around 0.05-0.1L/kg. After the slow distribution process reaches a steady state, the Vss is generally slightly larger at around 0.2 L/kg.
There are two ways for ADC drugs to cross the vascular wall to reach the interstitial fluid. One is filtration or convection across the vascular pores; After reaching the interstitial fluid, part of the drug binds to the target receptors on the membrane surface, and part returns to the venous system through the lymphatic circulation. In the process of circulation, ADC drugs may be metabolized by non-specific proteases, but the effect is generally weak. From the above process, it can be seen that the size of capillary pores and blood flow will affect the distribution of ADC drugs between tissues, generally showing that the distribution of heart, liver, spleen, lung and kidney is more. The properties of the ADC drug itself affect its distribution, except for the binding activity to the target mentioned above, the molecular size, charge and hydrophobicity of the ADC drug will affect its ability to cross capillary pores, especially after the payload is coupled. It will affect the distribution characteristics of naked antibodies. It has little effect when the DAR (drug-antibody ratios) is low. When the DAR value is greater than 4, it may lead to an increase in plasma clearance and the distribution of ADC drugs in the liver.
It is speculated that the excessive payload increases the overall hydrophobicity of the ADC, thereby making it easier to enter hepatocytes and hepatic macrophages through FcγR receptor-mediated phagocytosis or pinocytosis. In addition, the role of Fc receptors can also affect the distribution of ADC drugs. Fc receptors are mainly divided into two types: FcRn and FcγR receptors. FcRn is expressed in vascular endothelium, intestinal epithelium, blood-brain barrier, etc. FcRn-mediated endocytosis can help ADC drugs to cross these barriers. At present, there are few research examples in this area. If the mechanism is reliable, it will be beneficial to ADC drugs in the entity. tumor, especially in cases of brain metastases.
3 Elimination of ADC drugs
The elimination process of ADC drugs is relatively complex, and its structure consists of three parts. Therefore, when investigating the elimination of ADC, we need to disassemble it. The elimination mechanism of the antibody part mainly includes the target-mediated ADC elimination pathway, the neonatal Fc receptor pair The protective effect of antibodies, the protein stability of naked anti-self, etc.; at the same time, the cleavage of linker will also mediate the elimination of ADC, the main mechanisms include pH-dependent chemical degradation, cathepsin B, glutathione reduction of disulfide bonds, etc. , Many ADC linkers are non-cleavable types, the linker price is stable, and the release of the payload depends on the proteolysis of the antibody part into polypeptides or amino acids to release free small molecule toxins or small molecule toxin analogs with amino acid-linker. Finally, the elimination of ADC also needs to consider the elimination law after the payload is released, and can refer to the theory of common small molecule drugs.
3.1 Target-mediated elimination pathways
Target-mediated elimination refers to the specific binding of the ADC drug to the membrane surface antigen, and the antigen receptor-mediated endocytosis brings the ADC into the cell, and then is degraded in the lysosome. When the target-mediated elimination pathway is saturated, the target-mediated elimination pathway has obvious nonlinear PK characteristics. When it is not saturated, the amount of drug elimination per unit time is related to the drug concentration, showing the characteristics of first-order elimination kinetics. ; After reaching saturation, the elimination amount of the drug per unit time reaches the peak value and remains unchanged, showing zero-order kinetic characteristics. The rate of target-mediated elimination is affected not only by the expression of the target, but also by the rate of endocytosis of the drug-target complex. Although a higher endocytosis rate may accelerate the elimination of ADC drugs, the endocytosis mechanism is also a key step for ADC drugs to release toxins into cells to exert their efficacy, so we still hope that ADCs have a high endocytosis rate. Of course, the advantage of a higher endocytosis rate still requires sufficient target specificity as a premise, otherwise it will result in toxic side effects.
3.2 The role of FcRn receptors
The FcRn receptor has a protective effect on the elimination of the antibody part. After the ADC is endocytosed into the cell, the drug bound to FcRn will survive the degradation of lysosomes, and the binding of FcRn to ADC is pH-dependent. Under the condition of low pH of lysosome, the affinity of the two increases sharply to implement protection, and when ADC-FcRn returns to the cytoplasm with a high pH value, the affinity decreases and then the ADC drug is released. This mechanism also has nonlinear characteristics when FcRn receptor binding is saturated. This mechanism will prolong the half-life of ADC drugs in plasma and increase the ADCC effect mediated by ADC antibodies. At the same time, it should delay the payload release efficiency of non-cleaving linker ADC drugs, but it will not necessarily reduce the toxin-mediated efficacy. The role, in the end, must be combined with the PK/PD relationship. The strength of the protective effect of FcRn is largely determined by the affinity of ADC and the affinity of ADC to FcRn may be reduced if too much hydrophilic payload or PEG-modified linker is introduced.
3.3 Stability of Linker
At present, Linker is divided into cleavable type and non-cleavable type. The cleavable type means that the process of releasing the payload is mainly the uncoupling process of linker cleavage, while the non-cleavable type releases toxins or toxins similar to the catabolism of the antibody part. metabolites. The cleavable release methods are divided into chemical cleavage and enzymatic cleavage. Chemical cleavage uses the difference in pH between the blood and the target site to control the specific release of toxins, while enzymatic cleavage uses enzymes that are rich or specific in the target site. It acts to achieve specific release of toxins, such as lysosome-rich cathepsin B, intracellular glutathione reducing disulfide bond, phosphatase and pyrophosphatase, β-glucuronic acid plum, etc. For non-cleavable linkers, as long as the antibody part is stable enough, the content of free toxins in plasma, interstitial fluid, lymph and other parts can be reduced mechanically and the toxic and side effects can be reduced, but non-cleavable linkers need additional attention. Whether the formed toxin-amino acid/polypeptide still has strong cytotoxicity after hydrolysis.
Cleavable and non-cleavable linkers may cause differences in toxicity and efficacy due to different release products. The free toxins released by cleavable linkers have relatively higher permeability and can move back and forth freely. The free toxins in motion may affect the target tissue. Nearby cancer cells that do not express the target antigen play a killing effect, which is a bystander effect, and may also run to normal cells to cause toxic side effects; the release products of non-cleavable linkers are more toxin analogs connected to amino acid residues , its penetration is generally poor, and theoretically it will weaken the bystander effect and reduce the risk of side effects. Linkers with too high hydrophobicity can cause aggregation in plasma, increased plasma clearance, and hepatotoxicity due to increased hepatic uptake. Currently, the commonly used method is to introduce PEG or sulfonate into linker to balance its hydrophobic/hydrophilic properties. .
3.3 Dynamic Properties of Payload
After the payload is released, it is either confined to the release site due to poor permeability, or diffuses to other sites to play a role. The two types mentioned above have their own advantages and disadvantages in theory. In addition, many of the current payloads are substrates of efflux transporters such as P-gp, which may result in the formation of free toxins that are rapidly effluxed to the outside of the cell, resulting in loss of efficacy. If the role of P-gp is found in the study It significantly affects the content of intracellular toxins, and the factor hydrophilic group can also be used to increase the polarity of the linker-payload, weaken the affinity with the transporter protein, and avoid the efflux of P-gp.
The metabolism of Payload is also affected by common metabolic enzymes such as CYP. Although the content of Payload in the blood is extremely low under the premise that the linker is stable enough, it is still necessary to study the metabolism, excretion and DDI of Payload. It is important to understand the overall DMPK properties, PK/PD, PK/tox profiles of ADC drugs.