The Birth of ADC Drugs
In today’s anti-tumor treatment, many chemotherapeutic drugs have been found to have a killing effect on tumor cells. Unfortunately, chemotherapeutic drugs can not only kill tumor cells, but also attack normal human cells indiscriminately. Is there any way to maximize the attack on tumor cells while minimizing damage to normal cells? Under the guidance of such ideas, a new class of anti-tumor drugs was born—antibody drug conjugates.
The mechanism of action of ADC drugs
The design concept of antibody drug conjugate (ADC) has a long history. As early as 1913, Professor Paul Ehrlich, the father of chemotherapy and Nobel Prize winner, first proposed the concept of “magic bullet”, which means that cells Toxic drugs are mounted on specific monoclonal antibodies to achieve targeted killing of tumor cells. The ADC drugs currently on the market are based on this theory. By linking cytotoxic drugs to monoclonal antibodies, the monoclonal antibodies can be used as carriers to efficiently transport small-molecule cytotoxic drugs to target tumor cells in a targeted manner.
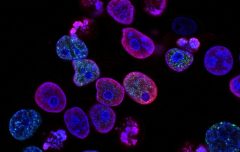
ADC drugs generally contain the following three key components: antibodies, linkers, and small-molecule cytotoxic drugs. After the ADC drug enters the blood, its antibody component can recognize the target and bind to tumor cells that highly express cell surface antigens. When the ADC-antigen complex enters tumor cells through endocytosis, the complex is degraded in lysosomes Under the action, the cytotoxic load (drug) will be released, destroy the DNA or organize tumor cell division, and play the role of killing tumor cells.
Clinical Use of ADC Drugs
The first generation of ADC drugs was an attempt in 1958 to use anti-mouse leukocyte immunoglobulin conjugated with methotrexate for the treatment of leukemia. Mylotarg is the first marketed ADC drug, which was approved by the FDA in 2000 for the treatment of acute myeloid leukemia, but was withdrawn from the market because Mylotarg produced severe and fatal liver damage and had no apparent survival benefit. The disadvantages of the first-generation ADC drugs are: the antibody is a mouse-derived antibody; Linker is not cleavable; the cytotoxicity is insufficient; the site is lowly expressed.
The starting point for the development of the second-generation ADC drug is trastuzumab, the first approved ADC drug targeting breast cancer. The most successful ADC in hematological oncology is Bentuximab, which targets classical Hodgkin lymphoma and anaplastic large cell lymphoma. The advantages of second-generation ADC drugs are: diversification of target antigen development; humanized antibodies; cleavable linker technology. The disadvantages are: the drug loading rate is too low or too high; the treatment window is narrow; the effectiveness is low.
The typical representative of the third-generation ADC drug is enrozumab, which is the second ADC drug targeting solid tumors and is suitable for patients with ineffective PD-1/PD-L1 antibody therapy. The advantages of third-generation ADC drugs are: small molecule-mAb site-directed coupling technology; development of bispecific antibodies; eukaryotic RNA splicing inhibitors to enhance specificity. Disadvantages are: coupling technology is difficult to reproduce; tubulin inhibitors are not sensitive.
At present, a total of 14 ADC drugs have been approved for marketing worldwide (12 FDA-approved, 1 China-approved, and 1 Japan-approved). In 2021, the FDA has successively approved the marketing applications of Zynlonta and Tivdak, the former being a CD19 ADC drug and the latter a TF ADC drug.
Epilogue
ADC drugs have shown excellent clinical efficacy in the fields of breast cancer, gastric cancer, urothelial cancer, lung cancer, and hematological tumors. It is believed that with the deepening of the understanding of ADC drugs by drug developers, the molecular structure design of ADC will be more reasonable. , the in vivo stability will continue to improve, thereby reducing toxic side effects, improving efficacy and activity, expanding the therapeutic window, and bringing new hope to tumor patients.