Since the beginning of May this year, monkeypox cases have been reported in non-endemic countries, and monkeypox cases have continued to appear in several endemic countries (West and Central Africa). In about four months (as of Sept. 7), the number of monkeypox patients soared to more than 54,000, with 18 deaths. The World Health Organization (WHO) declared the monkeypox outbreak a “public health emergency of international concern” on July 23. On September 6, the Centre for Health Protection of the Department of Health of the Hong Kong Special Administrative Region Government announced that the first imported case of monkeypox appeared in Hong Kong.
This article, combined with a recent review published in the journal Nature Reviews Immunology on September 5, describes the clinical, epidemiological and immunological characteristics of monkeypox virus infection and how to seize the opportunity to respond to the current monkeypox outbreak.
What is monkeypox
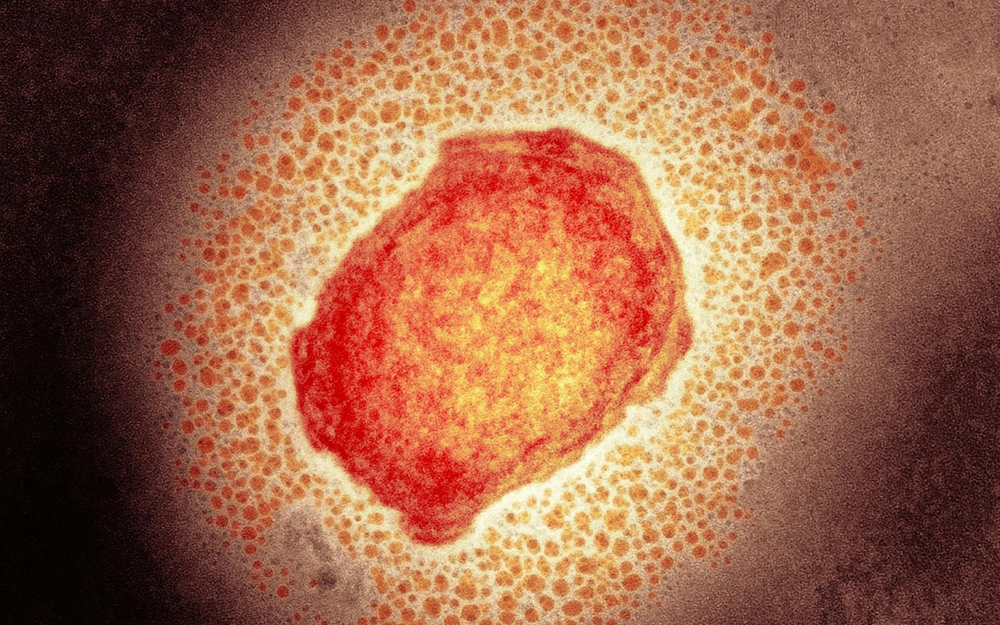
In 1958, a group of cynomolgus monkeys imported from Singapore to Denmark had an outbreak of vesicular disease, which was the first time the virus was discovered in humans, hence the name “monkeypox”. Monkeypox is a zoonotic infectious disease caused by monkeypox virus (MPXV), which belongs to the same genus of orthopoxvirus as smallpox virus.
Smallpox vaccine has been shown to protect against monkeypox: a 1988 Zaire study reported that people who were vaccinated against smallpox were about 85% less likely to contract monkeypox than unvaccinated people; in another study , found that vaccination made a difference in serious complications and long-term effects after MPXV infection (39.5% vs 74%), with a lower mortality rate in patients who received smallpox vaccine; a recent study on 528 cases diagnosed during the outbreak The infection study reported that only 9% of those infected had previously received the smallpox vaccine.
Therefore, the reason for the outbreak of monkeypox may be that the immunity of the general population to smallpox has declined, because in 1980, the WHO announced the eradication of smallpox, and after 1986, almost all countries in the world stopped smallpox vaccination.
monkeypox pathology
The incubation period for MPXV infection is 5-21 days, and common symptoms include fever (38.5-40.5°C), headache, and myalgia. A distinguishing feature of MPXV infection is enlarged lymph nodes in the upper jaw, neck, or groin (lymphadenopathy). Fever symptoms are followed by a rash that begins on the face, tongue, and mouth and spreads throughout the body. In the later stages of infection, lesions in the mouth can make drinking and eating difficult. However, recent monkeypox outbreaks have also reported some atypical clinical symptoms, including genital lesions in men who have sex with men (MSM) patients, with subsequent spread to other parts of the body, as well as the anus Ulcers, it appears that the distribution of skin lesions may be more limited than previously reported outbreaks.
The severity of the disease can be classified by the lesion count, since the higher the lesion count, the higher the risk of serious complications. Patients with severe complications may experience respiratory and gastrointestinal problems, encephalitis, sepsis, and eye infections, eventually leading to permanent vision loss. Skin lesions also increase the likelihood of bacterial infection of the skin, especially in patients who have not been vaccinated against smallpox.
The lesions typically go through four stages: macular, papule, vesicle, and pustule, and then fall off as a scab. Once the lesions have crusted over, the patient is generally considered non-infectious. However, it was reported that the scabs still contained large amounts of MPXV DNA 30 days after shedding, suggesting that infectious viral material may be present at this time. In addition, MPXV can also be transmitted vertically from the mother to the fetus during pregnancy.
A study conducted at Zaire in 1980-1985 reported a higher incidence of fatal disease in young children infected with MPXV, 14.9% in children aged 0-4 and 0% in children over 10, This difference may be due to differences in their immune responses.
Pathogenesis of MPXV
MPXV is a highly contagious orthopoxvirus, inhalation (inhalation of aerosolized respiratory secretions)/oral (intake of body fluids from an infected person) is a common route to establish a primary infection, the virus infects the oral and respiratory mucosa Later, the upper, middle, and lower epithelium of the respiratory tract are the main targets of primary infection. Infections at this stage are asymptomatic, with no signs of oropharyngeal lesions.
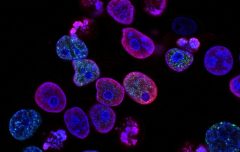
Virus transmission proceeds with infection of nearby tissue-resident immune cells, which may include antigen-presenting cells (eg, monocytes, macrophages, B cells, and dendritic cells). The mechanism by which orthopoxviruses transfer from the site of initial infection to nearby draining lymph nodes is a controversial topic: on the one hand, the transfer of dendritic cells from vaccinia virus (VACV)-infected mice from the lung epithelium to the draining lymph nodes may facilitated viral spread; on the other hand, VACV infection of human monocyte-derived dendritic cells proved infeasible, affecting dendritic cell maturation and its migratory potential, and opposing dendritic cell support Initial lymphatic spread of VACV. Importantly, however, VACV rapidly metastasized to draining lymph nodes within hours of inoculation, suggesting that direct entry of the virus into lymphatic vessels is a transmission mechanism.
Following infection of adjacent draining lymph nodes, orthopoxviruses replicate extensively in lymphoid tissue. Clinical studies have shown that lymphoid tissue in the neck and throat is the region where MPXV primary replicates. The tropism of MPXV in lymphoid tissues is associated with infection of monocytes/macrophages, dendritic cells, B cells, and activated T cells, which may also be targets of MPXV.
After the development of low-grade primary viremia caused by infection of lymphoid tissue, orthopoxviruses can spread to distant organs via the lymphovascular route. In the experimental mousepox model, the spleen and liver are the primary targets of infection after primary lymphatic dissemination, and viral infection in these organs releases a second major wave of viremia (thought to pass through infected cells) ), causing the virus to spread to the lungs, kidneys, intestines, skin and other organs.
The presence of orthopoxvirus in small dermal blood vessels marks the onset of skin infection and the development of skin lesions. However, how the virus reaches the upper layers of the skin, which lack blood and lymphatic vessels, is unclear. Importantly, epithelial lesions (herpes) also develop on the oropharyngeal mucosa, tongue, pharynx, larynx, trachea, and esophagus during MPXV infection, eventually developing into ulcers that release infectious viral particles into saliva.
In addition, infection can also occur through the skin. Dermal keratinocytes, fibroblasts, and tissue-resident antigen-presenting cells (eg, monocytes, macrophages, Langerhans cells, and dendritic cells) may become infected, and migrating antigen-presenting cells may contribute The virus spreads through the lymphatics.
Vaccine against monkeypox
Vaccines against smallpox have cross-protective activity against monkeypox, and the FDA has approved two vaccines for pre-exposure vaccination against orthopoxviruses including monkeypox: the second-generation live VACV vaccine ACAM2000 and the third-generation modified Ankara Vaccinia (MVA) attenuated vaccine JYNNEOS. Second-generation vaccines like ACAM2000 are the most common in the U.S. national stockpile, however these vaccines have several rare side effects, including myocarditis and pericarditis, that pose a higher risk to certain populations, such as those with eczema and pregnant women. Compared with earlier vaccines, third-generation attenuated vaccines such as JYNNEOS have better safety profile. However, because JYNNEOS is given two doses at 28-day intervals, in the case of post-exposure vaccination, the second dose may be too late to help prevent disease, and it is unclear whether the first dose is sufficient to achieve therapeutic effect.
A key to vaccine development is understanding the mechanisms by which different vaccines elicit immune responses, as different formulations can induce specific B-cell-mediated or T-cell-mediated immunity. Likewise, the immune capacity of the recipient and the route of immunization also affect the quality of the immune response. Given the frequent route of mucosal infection, specific induction of mucosal immunity may be critical in the context of MPXV. Another key need is to understand whether there is a risk of developing new strains of the virus when individuals infected with monkeypox are vaccinated. Co-infecting poxviruses can evolve by exchanging genetic information through homologous or non-homologous recombination.
How to treat monkeypox
Several treatments for smallpox are currently being developed for monkeypox, but the effectiveness of these treatments against monkeypox is based only on preclinical experiments and not supported by clinical data in humans.
The antiviral drug Tecovirimat does not affect the intracellular morphology of the virus (intracellular mature virus), but targets the VP37 membrane protein of MPXV, preventing the formation of enveloped virions, thereby disrupting the spread of the virus. Tecovirimat was effective in reducing monkeypox severity in a non-human primate (NHP) model, but its effectiveness decreased if treatment was given more than 5 days after viral infection. However, in one study, Tecovirimat was administered to one patient infected with monkeypox and had shorter viral shedding and disease duration compared to six untreated patients.
Another smallpox treatment is Brincidofovir, which inhibits orthopoxvirus DNA polymerase-mediated DNA synthesis and has shown efficacy against monkeypox in woodchuck and mouse models. In one human trial, three patients were treated with Brincidofovir, but all three were discontinued due to toxicity (increased liver enzymes). Cidofovir, the active pharmaceutical form of Brincidofovir, has also shown anti-poxvirus activity in in vitro and animal studies, but is nephrotoxic.
Summarize
Current studies on human systemic and mucosal immune responses during MPXV infection are limited, and a better understanding of the immune defense mechanisms of MPXV is needed. And it is unclear whether prior infection with VACV or MPXV or vaccination against smallpox induces any form of mucosal immunity. Given that MPXV and other poxviruses can be transmitted by respiratory aerosols, it is critical to characterize the mucosal immune response. Understanding the role of immunoglobulin A (IgA) and tissue-resident memory T cells in MPXV infection is particularly important and will provide a better understanding of MPXV-related respiratory complications. Likewise, foreskin mucosal immunity should also be characterized, as MPXV DNA has been identified in semen.
Defining the immunological correlates of protection is an important indicator for evaluating new vaccines, especially those targeting vulnerable groups of pregnant women and children. Currently, several countries, including the United Kingdom, the United States and Canada, have implemented Ring-fencing vaccinations to stop the potential spread of MPXV around the world. However, several challenges remain for successful vaccination: (1) not everyone is willing to receive the vaccine; (2) while currently available second- and third-generation vaccines are approximately 85% protective against MPXV in animal models , but their protective capacity in MPXV-infected humans remains unclear; (3) patients may be reluctant to initiate a diagnosis, given the current characterization of monkeypox in non-endemic areas as a disease primarily transmitted within the MSM community, especially in Countries where homosexuality is stigmatized or criminalized.
Many other infectious diseases are prevalent in Africa and may be co-infected with MPXV, such as alphavirus infection and malaria co-infection, which can significantly modulate host immunity and affect infection outcomes. Additionally, given the current MSM transmission in non-endemic countries, monkeypox and vaccination in the case of co-infection with other diseases in the MSM community are also needed, especially considering whether the patient is HIV-1 infected, as it can severely impair adaptation Sexual immune response.