Alzheimer’s disease (AD), commonly known as Alzheimer’s disease, is a global health problem with a high economic and social burden. There are approximately 50 million cases of dementia worldwide, with approximately 10 million new cases being added each year, and despite the efforts of the scientific community, there are still no very effective treatment options to prevent or cure Alzheimer’s disease.
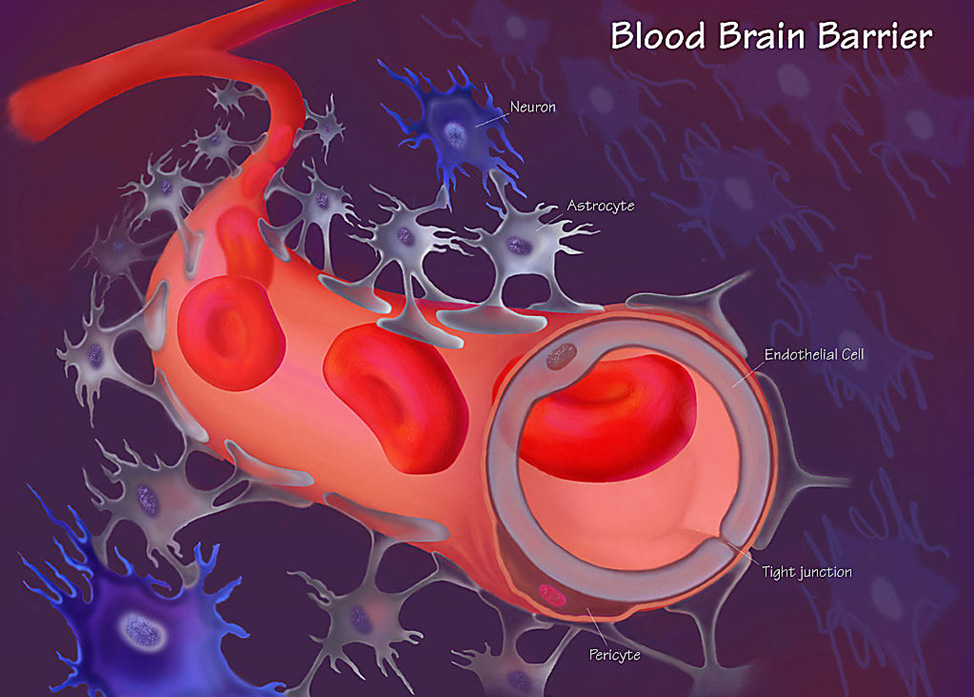
The blood-brain barrier, a layer of tightly packed cells that line the blood vessels of the brain, prevents toxins, pathogens and some nutrients from entering the brain and is an important evolutionary mechanism for the brain to protect the central nervous system from damage. Sadly, it’s also a major obstacle for therapeutic drugs to get inside the brain.
Recently, researchers from the University of Queensland School of Medicine in Australia published a research paper titled “Asporadic Alzheimer’s blood-brain barrier model for developing ultrasound-mediated delivery of Aducanumab and anti-Tau antibodies” in the journal “Theranostics”.
The study used focused ultrasound technology to open up a blood-brain cell model and deliver two Alzheimer’s-treating macromolecular drugs into the brain cell model, leading to entirely new therapies for the treatment of dementia.
Previously, the researchers used focused ultrasound combined with microbubble (FUS+MB) technology to cross the blood-brain barrier in animal models.
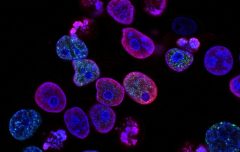
In the study, the researchers tested the method using stem cell cultures from Alzheimer’s patients to mimic the human blood-brain barrier, using stem cells from patients with apolipoprotein E4 and apolipoprotein E3 to grow a hemorrhagic brain cell model, The effects of focused ultrasound and microbubbles on the phenotype of blood brain cells were analyzed and two potential therapeutic Alzheimer’s antibodies were screened.
The study found that compared with the control cells, after treatment with focused ultrasound and microbubble technology, the blood-brain barrier was transiently opened in the blood-brain cell model. , the delivery increased significantly, up to 1.73 times.
In addition, the researchers demonstrated the safety of the method with little or no changes in the inflammatory response.
The researchers say this approach could be used as a personalized medicine approach, taking cells from patients and generating a blood-brain barrier model that can be tested to find the most suitable treatment.