Antibody-drug conjugates (ADCs) have achieved remarkable efficacy in cancer treatment and have attracted worldwide attention.
Although ADCs pose significant challenges to researchers, especially in identifying suitable combinations of antibodies, linkers, and payloads, 15 ADCs have so far been approved by the FDA.
Paul Ehrlich’s vision of targeted strategies to eliminate disease, whether microbes or malignant cells, has driven this research over the past century, notably creating a revolution in targeted cancer therapy.
In 1913, it was speculated that so-called “magic bullet” drugs could selectively destroy tumor cells through the use of toxins and targeting agents. More than 80 years later, Ehrlich basically realized this vision. With the successful development of chemotherapy drugs in the 1940s and the support of monoclonal antibodies (mAbs) in the 1970s, in 1983, the first successful antibody-drug conjugate (ADC ) Human clinical trials began. Administration safety and the ability of the conjugate to localize after radiolabeling were investigated in eight patients with advanced metastatic cancer.
While the feasibility of this approach was proven, several security issues were found, the most important of which was aggregation. ADCs are currently one of the fastest growing drug classes in oncology because they combine the best features of monoclonal antibodies and small molecule drugs to create a highly specific and cytotoxic holistic part of the therapy that is considered “Bio-missiles” for cancer treatment.
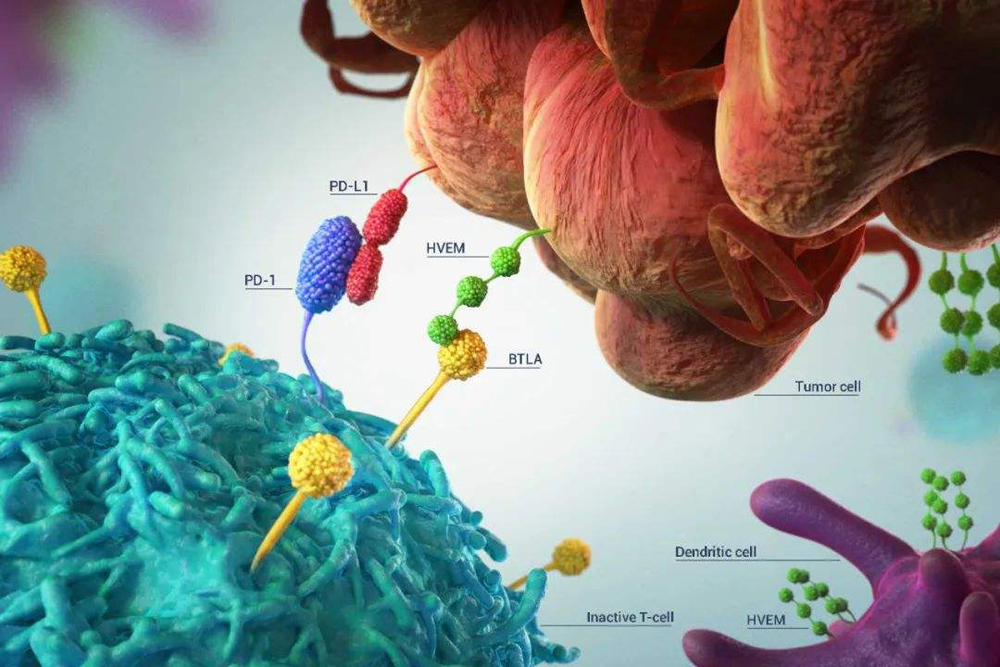
ADCs consist of three key elements: a monoclonal antibody that selectively binds to tumor cell surface antigens, a cytotoxic drug payload, and a cleavable or non-cleavable linker. Each of these components can make large differences between ADCs, resulting in great diversity in the overall structure and resulting in differences in the pharmacological and clinical properties of ADCs.
ADCs are designed to selectively deliver toxic payloads to cells expressing target antigens. Thus, target antigens that are preferentially expressed in tumor and non-malignant cells can be exploited to formulate a larger therapeutic window and reduce the phenomenon of off-target effects associated with the systemic effects of traditional chemotherapeutic drugs.
Antibody-drug conjugates(ADCs) list Approved by FDA(2000-2022)
The mechanism of action of ADC
The general mechanism of action of ADC is that after ADC is introduced into the plasma circulation, it recognizes a specific antigen on the surface of tumor cells and forms an antigen-ADC binding complex. The entire complex is then internalized, primarily through receptor-mediated endocytosis.
Inside early endosomes, some ADCs bind Fc receptors (FcRns) and undergo extracellular recycling. Following endosome maturation into late endosomes, the drug is released from the cleavable linker in the low pH environment of the lumen. Endosomes fuse with lysosomes, where the ADC and/or its components are exposed to proteolytic enzymes (e.g., cathepsin B), further facilitating payload release as the acidic environment increases. The free drug then causes cell destruction through a specific mode of action.
Most ADC payloads cause apoptosis through DNA damage or microtubule disruption. In addition, some payloads (those that are hydrophobic enough to cross the cell membrane and initially tethered to the antibody via a cleavable linker) can produce bystander effects. Free drug is exported from the target tumor cell and crosses the cell membrane to kill adjacent tumor cells, including those that may not express the relevant antigen on their cell surface or are inaccessible directly from the circulation.